RECOGNITIION, INSIGHT AND TARGETED CARE IN THE NTVG ABOUT PAIS?
Phew. I had secretly hoped to finally see a truly good article in the NTVG. Although I can appreciate that an attempt was made to describe the biology of post-acute infectious syndromes (PAIS), unfortunately this was once again a disappointing piece.
A few points stood out to me. Because of a registration problem I could not consult the references, so I had to guess which studies were being cited.
WHAT ABOUT M.E.?
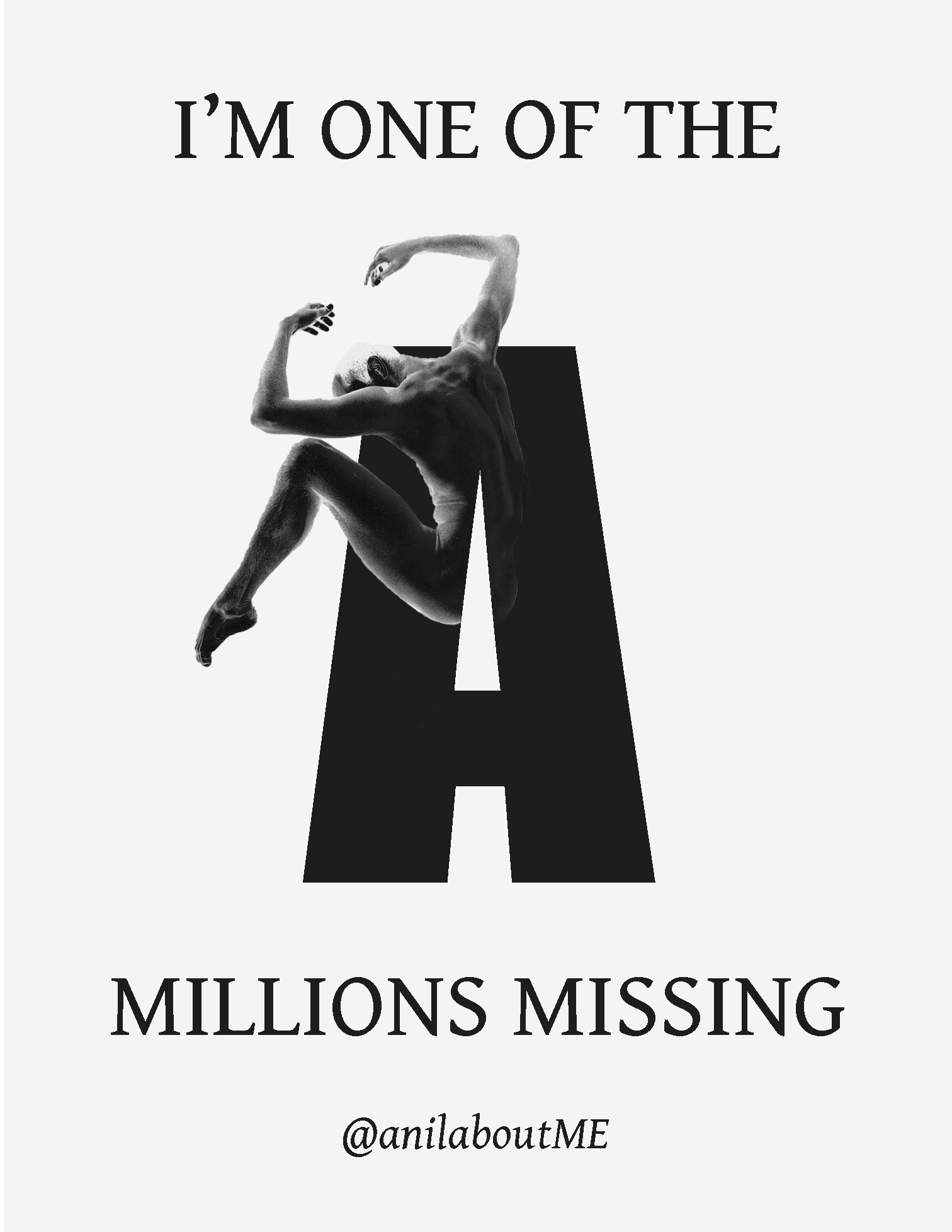
It is incomprehensible that an article about PAIS does not pay attention to ME. A significant proportion of people with PAIS meet the ME criteria, regardless of the original trigger. That means they in fact also have ME. An artificial separation is made with Long Covid, where post-exertional malaise (PEM) is mentioned, while PEM also occurs in other PAIS. PEM is the core symptom of ME. If you have PEM, you essentially also have ME. Ignoring this keeps the definitions and distinctions around PAIS unnecessarily vague. This does not help caregivers or patients.
The description of PEM is moreover very limited. Nothing is said about the delayed onset of PEM (12 to 72 hours after exertion), nor about the fact that it can involve both existing and new symptoms, often atypical compared to what one would expect after exertion.
In addition, the article chooses the tripartite division of physical, mental and emotional complaints. In the literature, however, the consistent terminology is physical, cognitive and emotional complaints. It is precisely physical and cognitive exertion that cause most symptoms. “Mental” is too broad and insufficiently specific.
RISK FACTORS?
The article states that anxiety and depression are risk factors for developing Long Covid. Although some studies suggest this, pre-infection data is often missing, which creates a distorted picture. The Lifelines study, which did have such data, found no significant association with psychiatric disorders:
“In contrast to previous studies, older age,9,10 smoking,9,10 cardiovascular disease, lung disease and psychiatric disorder9 were not significantly associated with post-COVID-19 condition, although point estimates for cardiovascular disease, lung disease and psychiatric disorder were increased.”
The focus on severe covid-19 as a risk factor is also not always correct. Many people experience it after a mild course.
DIAGNOSIS
Furthermore, it is stated that PAIS is a purely clinical diagnosis, without a specific test. That is true, but aspects such as post-exertional malaise and orthostatic intolerance (OI) can indeed be partly tested and objectified. For patients with ME and/or OI this provides a more positive and valid diagnosis. This should certainly have been mentioned. This should certainly have been mentioned more clearly. (1, 2)
BPS
The article suggests that BPS guidance for PAIS does not differ substantially from that for other chronic diseases such as cardiovascular disease or cancer. That sounds plausible, but has long led to problems.
For example, it is written: “Persistent complaints and limitations are usually accompanied by feelings of sadness, anger and powerlessness (the emotional dimension). This often leads to adjustments in functioning in various areas (the behavioral dimension).”
Although somatic dimensions are briefly mentioned, the emphasis is strongly on emotional and behavioral factors. This has been the case for years with PAIS. It is misleading, because it is precisely the biological dimensions such as PEM, orthostatic intolerance, MCAS-like symptoms, cognitive dysfunction, that cause most behavioral adjustments. The article, as written, gives the impression that the emotional dimensions are largely or primarily responsible.
Rehab
Through transdiagnostic diagnostics and cross-disease interventions, such as activity build-up in “chronic fatigue,” behavioral strategies have been deployed for decades that are harmful to people with PEM and ME. (1, 2, 3) This is not mentioned. Nor is the fact that internationally there is increasing distance from these forms of psychotherapy and rehabilitation.
It is therefore important to make clear distinctions in how people can best be supported psychosocially. Instead of interventions such as cognitive behavioral therapy (CBT) and graded exercise therapy (GET) that are based on fatigue and activity build-up, it is essential to focus on interventions based on biological factors and PEM through pacing and staying within one’s own limits, without gradually increasing activy levels. These articles align better with that approach:
Unfortunately, the article also refers to the review by Zeraatkar et al. (2024), which presented CBT and rehabilitation as effective for Long Covid. As Tuller et al. stated in their letter to the BMJ, this concerned patients with acute covid who had been hospitalized. This cannot simply be extrapolated to everyone with Long Covid, and certainly not to patients with an ME-like PEM phenotype. Vink et al. came to similar conclusions.
The CBT study by Kuut et al. (2023) moreover showed no objective improvements. This was not mentioned, which creates an overly positive picture of CBT and rehabilitation in Long Covid-ME patients.
The article does mention that antibiotics were not effective in QVS, but omits that CBT in the Qure study also did not lead to objective improvements and that any effects disappeared at follow-up. Not mentioning this is also misleading.
B(P)S
Finally, the text states that distress and “catastrophic” thoughts probably predict a worse course. Reference .24, however, is about MUPS and the reference in that article is about chronic fatigue in general practice, not specifically about PAIS. PAIS is not the same as chronic fatigue.
It suggests a causal relationship, while distress can also be a consequence of persistent complaints. Moreover, no distinction is made between phenotypes, while in some natural recovery is much more likely.
Catastrophic thoughts can be rational in the context of severe, disabling symptoms such as ME or Long Covid. Pathologizing them leads to victim blaming, and this article does that implicitly.
Almost all authors are members of the Health Council committee for Long Covid. If this article forms the basis for the upcoming advice, that is cause for serious concern for both physicians, other caregivers, and people with PAIS. The risk is that PAIS and Long Covid will be misinterpreted, causing physicians to unintentionally inflict iatrogenic harm. Patients then not only risk having their complaints dismissed, but also not receiving the appropriate medical care they need and potentially suffering harm.
It is particularly disappointing that the NTVG once again fails to publish a current, scientifically well-founded article on PAIS. That this piece appeared in this form genuinely surprises me.
Although there are certainly elements that are correct, the article also contains several parts that are outdated, misleading or insufficiently substantiated. For a journal that should represent the medical standard, this level is extremely problematic. How is this the standard of the NTVG?
This article certainly does not provide the hoped-for recognition, insights and targeted care. Unfortunately, it only creates more confusion and potential harm.